Differential Red Eye Diagnosis ~ LINK
Red Flags
- Pain
- Reduced vision
- Photophobia
- Haloes around lights
- CL wearer
- Cold sores ~ HSV-1
 | ||
 | ||
 |
| Redness | Pain | VA | Lacrimation | Photophobia | Other | Investigate | Action | Referral | |
Subconjuntival Haemorrhage | Blood red Localised | Little or none | Unaffected | None | None | None | If occurred before then check BP | Reassure | Not for isolated occurances |
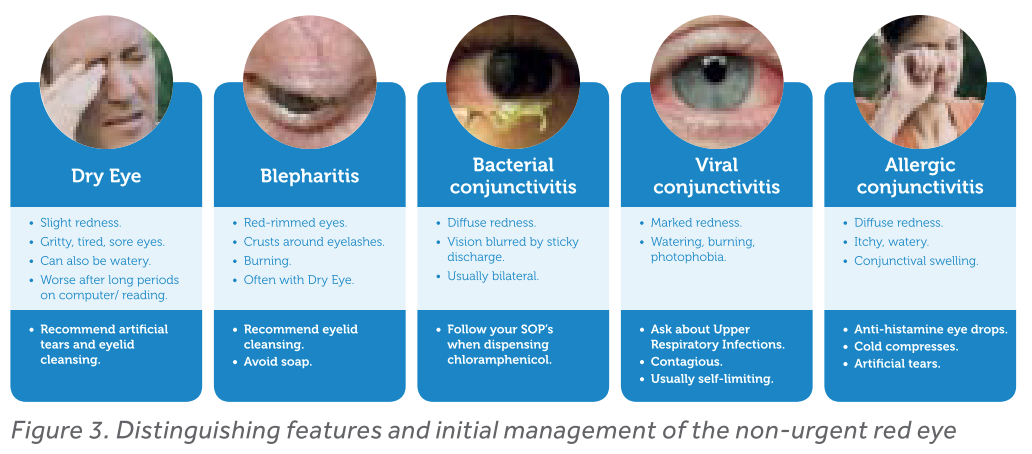
| Conjuctivitis(Bacterial) | Conjunctival, at inner and outer canthi | hot, gritty, sore, itchy | Unaffected | None or mild | Yes | Yellow discharge. Eyelids stuck together on waking | Ask if other family members are affected | No CL wear. Avoid sharing face towels | Consult GP if bad |
| Conjunctival at inner and outer canthi and will last 2-3 weeks | Discomfort | Normaly unaffected, but on rare instances it can be blurry, or glare when looking at lights | Watery | Artificial tears & painkillers. Regular lid cleaning and cold compresses | GP only if severe for steroid. Conjunctivitis is contagious and spreads very easily by water droplets (coughing, sneezing) or contact with tissues, flannels, towels, pillowcases and so on. For that reason, it’s really important to wash your hands frequently and dispose of tissues after use to prevent the condition from spreading to other family members or work colleagues | ||||
| Conjunctivitis(Allergic) | Conjunctival | Itchy | Unaffected | Yes | None | May have runny nose, sneezing | Opticrom, anti-hist drops or tabs. Cold compress. Don't rub | Rarely. Only if severe and not responding to treatment | |
| Iritis (Acute) | Limbal | Moderate to severe | Reduced | Yes | Yes | Irregular pupil shape when dilated | Aqueousflare, keratitic precipitates | See OO. Instill mydriatic | Urgent HES |
| Sometimes | Usually out of proportion. Sometimes FB sensation. 5% no pain | Usually drops | Yes | Yes | Discharge | Early signs are mild and non-speciific | Later signs include stromal infiltrates (ring-shaped, disciform, or numular), satellite lesions, epithelial defects, radial keratoneuritis, scleritis, and anterior uveitis (with possible hypopyon). Advanced signs include stromal thinning and corneal perforation | Refer as soon as suspected | |
Keratitis, Ulcerative (sterile, culture negative) | Limbal or generalised | Minor to moderate FB sensation | Can be affected | Yes | Yes, may be severe | Corneal lesion, stains with fluoro | Stop CL wear Prophylactic topical antibiotic Review in 24 hours. Refit with dailies | If in doubt as to sterile or infectious, then treat as infective
| |
| Generalised | Increasing | Can reduce | Yes | Yes | Anterior chamber cells and flare and mucopurulent discharge can be present | See above
Consider differntial diagnoses | Broad spectrum antibiotic: Chloromycetin, Optrex Infected Eye Drops or Optrex Infected Eye Ointment | Judged based on size, location, VA and other symptoms/signs | |
| Keratitis, Fungal | Generalised | Notable, or FB sensation | Reduced | Yes | Yes | Yellow, purulent | white/gray infiltrate with feathery borders. Can mimic MK | Refer | |
| Diffuse conjunctival and limbal hyperemia | Sudden onset, unilateral | Unaffected | Yes | Yes | Multiple corneal epithelial and subepithelial infiltrates (periphery and mid-periphery) | In more severe cases of CLARE, corneal edema or anterior uveitis may also be present (rare) | Associated with sleeping & napping, also upper respiratory tract infections are associated with gram-negative organisms like Haemophilus influenza (100x) | Self-limiting. Cease CL wear. Use artifical tears. | |
| Episcleritis | Diffuse or sectoral, bright red or pink bulbar injection, unilateral | Discomfort or tenderness | Unaffected | Sometimes | Sometimes | Eyelid edema and conjunctival chemosis may be present | No discharge | Artificial tears and Ibuprfuen | Self-limiting Peaks after 12 hours Subsides after 2-3 days
Refer to GP is reoccurs often |
The superficial vessels appear straight and are arranged in a radial fashion. The deeper visceral layer contains a highly anastomotic network of vessels
The area of injection should be examined with the slit lamp. If the examiner uses a narrow, bright slit beam, nodular episcleritis can be distinguished from scleritis. In nodular scleritis, the inner reflection, which rests on the sclera and visceral layer, will remain undisturbed while the outer reflection will be displaced forward by the episcleral nodule. In scleritis, both of light beams will be displaced forward. Also important to note is that the nodule in episcleritis is freely mobile over the scleral tissue that lies underneath.
In practice, the differentiation of episcleritis and scleritis is often aided by the instillation of phenylephrine 2.5%. The phenylephrine blanches the conjunctival and episcleral vessels but leaves the scleral vessels undisturbed. If a patient's eye redness improves after phenylephrine instillation, the diagnosis of episcleritis can be made. According to Krachmer et al, phenylephrine 2.5% eye drops blanch conjunctival vessels, allowing the differentiation of conjunctivitis and episcleritis. Instillation of phenylephrine 10% will result in blanching of the superficial episcleral vascular network but not the deep plexus, thus distinguishing between episcleritis and scleritis. | |||||||||
| Scleriris | Violet-bluish hue with scleral edema and dilatation | Severe but dull, may include orbit, sometimes ear, scalp, face and jaw. Worse with eye movement. Worse at night, may wake Px | Can be seriously affected | Yes | Yes | May be keratitis with infiltrates. uveitis, and trabeculitis
Many non-ocular signs. CLICK LINK | Consider differential diagnosis | Refer HES | |
Scleritis presents with a characteristic violet-bluish hue with scleral edema and dilatation. Examination in natural light is useful in differentiating the subtle color differences between scleritis and episcleritis. On slit-lamp biomicroscopy, inflamed scleral vessels often have a criss-crossed pattern and are adherent to the sclera. They cannot be moved with a cotton-tipped applicator, which differentiates inflamed scleral vessels from more superficial episcleral vessels. Red-free light with the slit lamp also accentuates the visibility of the blood vessels and areas of capillary nonperfusion. Finally, the conjunctival and superficial vessels may blanch with 2.5-10% phenylephrine but deep vessels are not affected. The globe is also often tender to touch. | |||||||||
FB | Generalised | Sharp, sudden onset | Probably unaffected | Yes, marked | Yes, marked | Blepharospasm | Evert lid. Look for tracker stain | Flush with saline | Hospital if still present |
| Acute Closed Angle Glaucoma | Generalised, limbal | Severe, may cause nausea | Reduced | No | No | Cloudy cornea. Dilated oval pupil, unresposive to light | Raised IOP | See OO. Instill miotic | Urgent HES |
Microbial and Sterile Infiltrative Keratitis
MK. Sight threatening.
~ A positive corneal culture or a corneal infiltrate and overlying epithelial defect with one or more of the following signs
~ Any part of the lesion within or overlapping the central 4mm of the cornea
~ Uveitits
~ Pain
Inpoertant Diagnostic Factors
~ Any anterior chamber activity (with or without hypopyon
~ corneal staining
~ conjunctival injection (circumferential in severe cases but more sectorial in less severe cases)
~ Size, location, depth, shape and colour of the lesion
Reported symptoms
~ pain
~ photophobia
Occurs
~ superiorly with CW silicone wear
~ peripherally with hydrogels
~ centrally with daily disposable
Equal threat whatever the soft lens type, perhaps slightly less with dailies when worn correctly.
Notes
Round lesions are CLPU
Oval lesions are marginal keratitis