B&L RGP Varifocal LINK: B&L fitting guides
Ensure no CL wear for 2/365 to take accurate K's
Provide B&L with K's, and spec Rx
The CL add will be +0.50 stronger than the spectacle add
The lens should move 2mm with downgaze
Fitting Principles
Although these lenses may be empirically fit, the best success has been found when they have been fit using diagnostic (trial) lenses. There are no conversion requirements or special techniques required for fitting this multifocal design. The following guidelines have been provided to maximize the fitting success of the lens.
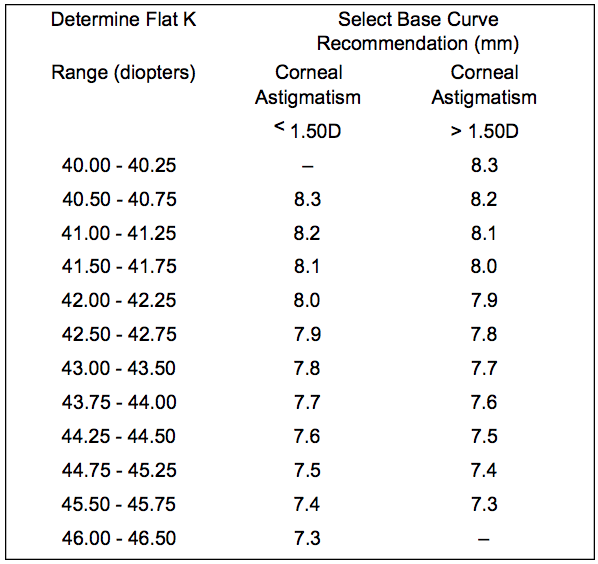
Initial Base Curve Selection:
If the patient’s corneal cylinder is less than or equal to 1.50D, then the initial base curve selected should correspond to the patient’s flat K reading.
If the patient’s corneal cylinder is greater than 1.50D, the initial base curve selected should correspond to 0.1 to 0.2 mm steeper than the patient’s flat K reading.
In general, the goal of the fit of this multifocal design is to achieve good centration of the lens over the pupil, although superior central position may also be acceptable.
The lens must translate well with the blink (1-2 mm) ensuring that the reading portion of the lens moves over the pupillary area upon down gaze. The patient should be instructed to keep their head erect while moving their gaze to an inferior position (much like progressive addition multifocal spectacle lenses) to maximally utilize the reading portion.
Example:
Step one: Measure central corneal curvature and identify the Flat K (lowest dioptric power)
In this example – K = 42.75/44.75 @ 90;Flat K = 42.75D (7.90mm) The “Flat K”is used as a reference point from which the Base Curve Radius is Chosen.
Step two: Calculate the corneal astigmatism (difference between the flat and steep K).
In this example – K = 42.75/44 .75 @ 90;Corneal Astigmatism = 2.00D
Step three: Calculate the Base Curve Radius. In this example – K = 42.75/44.75 @ 90; Flat K = 7.90D Corneal Astigmatism = 2.00D Lens Diameter = 9.6 mm Initial Base Curve: Flat K 42.75D 7.90mm + Corneal Astigmatism Factor 0.50D steeper than Flat K = Initial Base Cur ve 43.25D Base Curve Radius 43.25D 7.80 mm
You may use the above method to select your initial base curve or you may refer to the chart below: Note: Corneal astigmatism greater than 1.50D should be evaluated with a 0.1 mm steeper lens. Greater than 2.50D of corneal astigmatism may require a 0.2 mm steeper lens.
With this initial base curve selection evaluate the following:
A. Lens Movement:
The lens MUST move freely with the blink. Poor translation will not place the reading portion of the lens in front of the pupillary zone upon down gaze. If the lens does not translate well, try a flatter base curve.The greatest effect of the add is achieved when the lens interacts with the lower lid in down gaze which will facilitate upward translation
B. Lens Centration:
The lens should center over the pupil in primary gaze and translate upward in down gaze. The greatest effect of the add is achieved when the lens interacts with the lower lid in down gaze which will facilitate upward transla - tion.If the lens is not well centered over the pupil in primary gaze (straight ahead) try a steeper base curve.
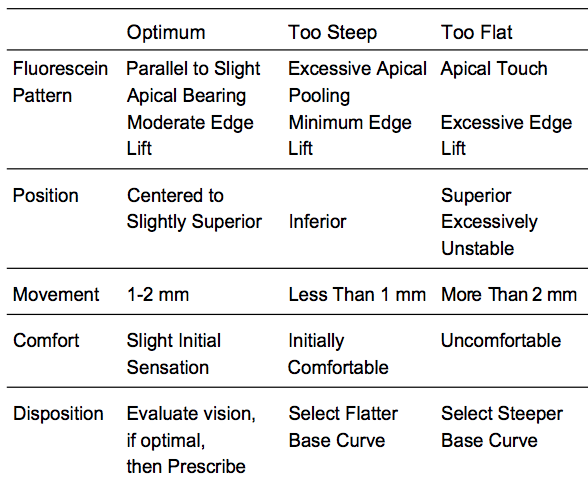
C. Fluorescein Pattern:
In evaluating the fluorescein pattern, divide the pattern into three zones: central, intermediate and peripheral. The ideal fluorescein pattern is one that demonstrates an aligned to slightly bearing central zone, an aligned intermediate zone and a peripheral zone that demonstrates a slightly high edge. This slightly high edge lift or fluorescein pooling, is normal as long as there is not an excessive amount of edge lift, i.e., creating bubble formation at the edge or causing the lens to be unstable.
The presence of the UV-absorber in the BOSTON® MultiVision (enflufocon A) contact lens may require equipment enhancement to visualize fluorescein patterns adequately. A simple, inexpensive approach is the use of an auxiliary yellow Kodak Wratten #12 filter in conjunction with the cobalt blue filter of the biomicroscope.
Slit Lamp Application:
1. All customary light intensities and filter settings (Cobalt Blue) are left in place.
2. The Kodak Wratten Filter #12* (yellow) is secured on the patient side of the slit lamp microscope with a small piece of adhesive tape.
Optimizing Visual Performance:
After an acceptable fluorescein pattern is achieved, further base cur ve adjustments may still be required to optimized visual performance.
Use the above fitting guidelines to achieve an optimum fit. Place the distance spherical over-refraction in a trial frame and measure the distance and near visual acuities. Use full room illumination at near, and record acuity to the single letter. If you have excellent distance visual acuity, and less than Jaeger 1 (J1) at near, continue the trial fitting to optimize near vision.
Fit 0.1-0.2 mm Flatter If:
• The lens does not have enough interaction with the lower lid in down gaze to move the lens upward.
• In down gaze, the lens binds to the superior cornea, preventing it from maximal translation. (Lift the upper lid while the patient moves from primary gaze to down gaze to make this assessment).
• The fluorescein pattern shows significant central pooling.
Fit 0.1-0.2 mm Steeper If:
• Lid attachment causes the lens to mo ve to an excessively superior position.
• The lens decenters nasally or temporally
• The fluorescein pattern shows significant central bearing.
The key to diagnostic fitting is primarily the patient’s visual response. Order the base curve that provides the maximal distance and near vision with an acceptable overall fit based on fluorescein pattern interpretation.
Initial Lens Power Selection
Step 1: Perform a spherical refraction over the best-fitting trial lens.
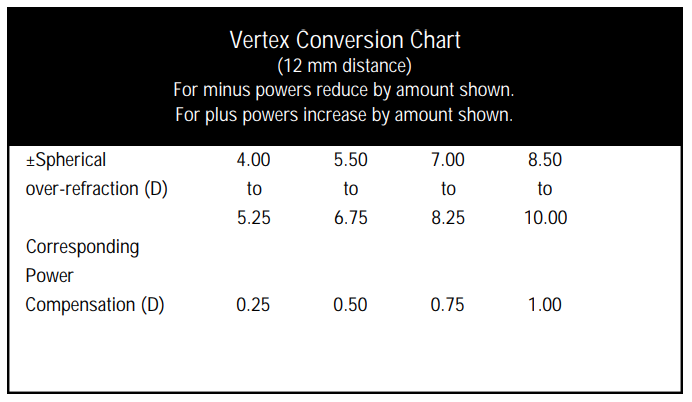
Step 2: If the spherical power of the over-refraction is greater than 4.00D, correct for the vertex distance.
Example: -5.00D at 12 mm =-4.75D at the cornea +5.00D at 12 mm= +5.37D at the cornea
Step 3: Combine the spherical over-refraction (corrected for vertex distance if appropriate) with the power of the trial lens to obtain the final contact lens power ordered.
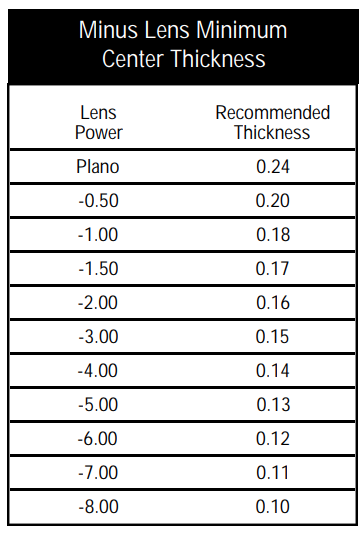
Initial Lens Center Thickness Selection For best clinical results, your Authorized BOSTON® Manufacturer will manufacture each BOSTON MultiVision contact lens with an optimal center thickness. If you choose to specify center thickness, we do not recommend center thicknesses for minus lenses below the following minimums:
Remaining Lens Parameter Selection
The final prescription should be provided to the Authorized BOSTON®Manufacturer in a format which includes:
• base curve
• center thickness
• diameter of 9.6mm
• distance power
RECOMMENDED INITIAL WEARING SCHEDULE
The maximum suggested wearing time for these lenses is:
| DAY | Wearing Time (Hours)* |
| 1 | 4 to 8 hours |
| 2 | 6 to 10 hours |
| 3 | 8 to 14 hours |
| 4 | 10 to 15 hours |
| 5 | 12 to all waking hours |
| 6 | All waking hours |
*if the lenses continue to be well-tolerated
CLINICAL ASSESSMENT
1.Criteria of a Well-Fitted Lens Patient comfort is largely determined by lens positioning on the cornea.
A central or slightly superior, lid attachment positioning is generally preferred to enhance comfort and maximize lens performance.
Inferior lens positioning, which interferes with normal blinking and promotes lens binding and 3-9 staining, as well as poor multifocal visual performance should be avoided.
Ideally, the fluorescein pattern of the lens should demonstrate alignment without excessive peripheral bearing. Excessive apical pooling or bearing should be avoided.
A moderate edge lift is necessary to permit the edge of the lens to slide over the corneal surface with minimal resistance.
2.Optimizing Fitting Characteristics In order to achieve optimal performance, it is often necessary to modify the initial trial lens parameters. Practitioner observations and interpretation of lens positioning, fluorescein patterns, and lens movement are essential to this process. The following chart summarizes common fitting relationships.
3.Problem Solving
Persistent excessive lens awareness: This problem may be due to:the use of incompatible care products; improper use of care products (i.e., lens cleaning just prior to insertion);three and nine o’clock staining; deposits on the concave lens surface;accumulation of mucus under the lens;poor edge design, incomplete blinking or steeply fitted lenses.
Three and nine o’clock staining:If the lens positions low, it should be refit to achieve a higher position so as to avoid a false blink pattern.Complete blinking should be encouraged.
Generalized corneal staining:In cases of diffuse staining not apparently related to back surface deposits on the lens, solution or preservative incompatibility should be ruled out.
Ocular redness without staining:This problem may be caused by some component of the care solutions such as preservatives or the presence of pingueculae, infectious or allergic conjunctivitis, or inadequate lens lubrication, including excessive mucus accumulation as occurs in dry eyes.
Excessive development of lens deposits:This unusual problem may be related to:increased mucus production, i.e., GPC, keratitis sicca, chronic allergies, etc.The more frequent use of the BOSTON® Rewetting Drops may be helpful in these cases. In most cases, deposits are easily removed by cleaning with original BOSTON® Cleaner or BOSTON Advance® Cleaner. In the event that deposits cannot be removed by cleaning the lens should be replaced.
Lens surface dry spots:
The presence of discrete non-wetting areas on a new or recently modified or polished lens are usually due to the persistence of hydrophobic products used during lens fabrication. These hydrophobic contaminants have a greater affinity for BOSTON®ES (enflufocon A) polymers and if not removed with the BOSTON® Laboratory Lens Cleaner, the lenses should be returned to the Authorized BOSTON® Manufacturer for a special solvent cleaning. Other causes of loss of surface wettability include:surface contamination with cosmetics, hair spray, skin preparations;inadequate tear lubrication;incomplete blinking;the use of incompatible preserved care solutions;and dry lens storage. Recurrent lens warpage:This may be due to repeated, excessive compression of lenses during handling (especially low-minus lenses having a less-than-recommended center thickness) or excessive flexing of minus lenses on astigmatic corneas. Carefully reviewing the proper technique for lens handling and increasing the center thickness by 0.02 to 0.04 mm to reduce lens flexure will minimize recurrent lens warpage. Unstable vision:This problem may be due to excessive blink-induced lens flexure resulting from a steep fit. Unstable vision may also result from excessive blink-induced lens movement. Reduced contact lens-corrected vision:Reduced vision correction unrelated to changes in refractive error may be due to lens warpage, front surface deposits, or switched lenses. Repeated lens breakage: Lens breakage problems may be due to careless handling or storage procedures (see Patient Instructions booklet) or the use of lenses having less-than-recommended center, edge or junction thickn e s s, especially for patients having poor manual dex t e ri t y. MODIFIEDMONOVISION FITTING TECHNIQUE* For BOSTON® MultiVision the definition of modified monovision is where one lens is corrected in the normal manner (full correction for distance) while the other lens is prescribed with a slight amount of plus power (+0.5D to +0.75D) over the normal distance correction.This additional plus power should increase near vision acuity in that eye and overall. *A mild over correction of +0.50 diopters will enhance the near nominal add without degrading the distance vision significantly. NOTE: Modified Monovision correction should not be used when it is in conflict with the visual requirements for federal or state licensing. 1. Patient Selection A.Modified Monovision Needs Assessment For a good prognosis the patient should have adequately corrected distance and near visual acuity in each eye. The amblyopic patient may not be a good candidate for modified monovision with the BOSTON® MultiVision (enflufocon A) Contact Lens. Occupational and environmental visual demands should be considered.If the patient requires critical vision (visual acuity and stereopsis), it should be determined by trial whether this patient can function adequately with modified monovision.Modified monovision contact lens wear may not be optimal for such activities as: (1) visually demanding situations such as operating potentially dangerous machinery or performing other potentially hazardous activities;and (2) driving automobiles (e.g., driving at night). Patients who cannot pass their state drivers license requirements with modified monovision correction should be advised not to drive with this correction, OR may require that additional over-correction be prescri b e d . B. Patient Education All patients do not function equally well with modified monovision correction. Patients may not perform as well for certain tasks with this correction as they have with bifocal reading glasses. Each patient should understand that modified monovision, as well as other presb yopic contact lenses, or other alternatives, can create a vision compromise that may reduce visual acuity and depth perception for distance and near tasks. During the fitting process it is necessary for the patient to realize the disadvantages as well as the advantages of clear near vision in straight ahead and upward gaze that modified monovision contact lenses prov i d e. 2.Eye Selection Generally, the nondominant eye is corrected for near vision.The following test for eye dominance can be used. A.Ocular Preference Determination Methods Method 1 - Determine which eye is the "dominate eye." Have the patient point to an object at the far end of the r o o m .C over one eye. If the patient is still pointing directly at the object, the eye being used is the dominant (sighting) eye. Method 2 - Determine which eye will accept the added po wer with the least reduction in vision.Place the appropriate plus power trial spectacle lens in front of one eye and then the other while the distance refractive error correction is in place for both eyes. Determine whether the patient functions best with the plus power trial lens over the right or left eye. B.Refractive Error Method For anisometropic corrections, it is generally best to fit the more hyperopic (less myopic) eye for distance and over-plus the more myopic (less hyperopic eye) to increase near correction. C.Visual Demands Method Consider the patient’s occupation during the eye selection process to determine the critical vision requirements. If a patient’s gaze for near tasks is usually in one direction, correct the eye on that side for near. Example: A secretary who places copy to the left side of the desk may function best with the near lens on the left eye. 3.Near Add Determination Always prescribe the lens po wer for the near eye that provides optimal near acuity at the midpoint of the patient’s habitual reading distance. However, when more than one power provides optimal reading performance, prescribe the least plus (most minus) of the powers. 4.Trial Lens Fitting A trial fitting is performed in the office to allow the patient to experience modified monovision correction. Lenses are fit according to the directions in the general fitting guidelines and base curve selection described earlier in the guide. Case history and standard clinical evaluation procedure should be used to determine the prognosis. Determine which eye is to be corrected for distance and which eye is to be corrected for near. Next, determine the appropriate amount of additional plus power for the near vision eye.With trial lenses of the proper power in place, observe the reaction to this mode of correction.Immediately after the correct power lenses are in place, walk across the room and have the patient look at you.Assess the patient’s reaction to distance vision under these circumstances.Then have the patient look at familiar near objects such as a watch face or fingernails. Again assess the reaction.As the patient continues to look around the room at both near and distance objects, observe the reactions. Only after these visual tasks are completed should the patient be asked to read print.Evaluate the patient’s reaction to large print (e.g.typewritten copy) at first and then graduate to news print and finally smaller type sizes. After the patient’s performance under the above conditions is completed, tests of visual acuity and reading ability under conditions of moderately dim illumination should be attempted. An initial unfavorable response in the office, while indicative of a guarded prognosis, should not immediately rule out a more extensive trial under the usual conditions in which a patient functions